Post-Traumatic Stress Disorder, or PTSD, is a serious mental health condition that can develop in individuals who have experienced or witnessed a terrifying, shocking, or dangerous event. While it is widely associated with military combat, PTSD can affect anyone, at any age, following a wide range of traumatic experiences, including natural disasters, serious accidents, physical or sexual assault, or the sudden death of a loved one. The condition is characterized by a persistent and distressing set of symptoms that emerge after the trauma, significantly interfering with a person’s daily life, relationships, and overall well-being. Understanding PTSD is the first step toward recognizing its signs and seeking the effective, evidence-based treatments that can lead to recovery.
Understanding the Traumatic Event
At the core of PTSD is a traumatic event, often called a “stressor.” This is an experience that overwhelms a person’s ability to cope, creating intense feelings of fear, helplessness, or horror. The types of events that can lead to PTSD are broad and deeply personal.
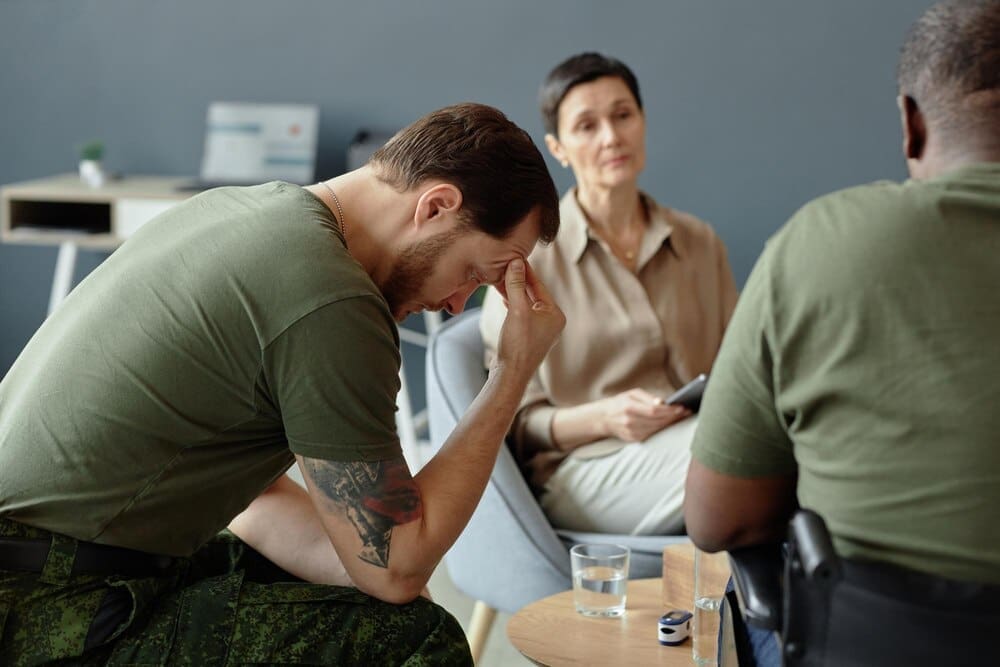
Common examples include direct exposure to violence, such as being a victim of assault, domestic abuse, or a terrorist attack. Witnessing such events happen to others can be equally traumatic. First responders, like paramedics and police officers, and military personnel are at a higher risk due to their frequent exposure to life-threatening situations.
However, trauma is not limited to violence. Surviving a severe car crash, a natural disaster like a hurricane or earthquake, or receiving a life-threatening medical diagnosis can also trigger PTSD. For children, experiences like physical, emotional, or sexual abuse, or neglect, are potent stressors that can have lasting effects.
It is crucial to understand that the objective severity of an event does not solely determine whether someone will develop PTSD. A person’s subjective experience—their personal perception of the threat and their emotional response—is what matters most. What is profoundly traumatic for one person may not be for another.
The Core Symptoms of PTSD
The symptoms of PTSD are grouped into four main categories. For a diagnosis to be made, a person must experience symptoms from all four clusters for at least one month, and these symptoms must cause significant distress or problems in their daily functioning.
Intrusion and Re-Experiencing
Perhaps the most well-known symptom of PTSD is the way the trauma persistently intrudes into a person’s present life. This is not simply remembering a bad event; it is reliving it in a visceral and distressing way.
This can manifest as unwanted, upsetting memories that surface unexpectedly. Many people with PTSD experience vivid and terrifying nightmares about the event. The most intense form of re-experiencing is a flashback, where a person feels or acts as if the traumatic event is happening again in that very moment, losing touch with their current surroundings.
Individuals may also experience intense emotional distress or physical reactions—like a racing heart, sweating, or nausea—when they encounter “triggers,” which are internal or external cues that remind them of the trauma. A car backfiring might trigger a combat veteran, while a specific scent or location might trigger a survivor of assault.
Avoidance
To cope with the pain of re-experiencing the trauma, individuals with PTSD often go to great lengths to avoid anything associated with it. This avoidance can take two forms.
First, they may try to avoid internal reminders, such as thoughts, feelings, or memories related to the event. They might refuse to talk about what happened or push the memories out of their mind. Second, they actively avoid external reminders, such as people, places, activities, or situations that could trigger distressing memories. A person who was in a serious car accident, for example, might stop driving altogether.
While this avoidance provides temporary relief, it ultimately reinforces the fear and prevents healing. Over time, it can cause a person’s world to shrink, leading to social isolation and a loss of connection to activities they once enjoyed.
Negative Alterations in Cognition and Mood
Trauma can fundamentally change how a person thinks about themselves, others, and the world. This cluster of symptoms involves a persistent and distorted set of negative beliefs and emotions.
Many people struggle with memory, often unable to recall important aspects of the traumatic event. They may develop deeply ingrained negative beliefs, such as, “I am bad,” or “The world is completely dangerous.” It is also common to experience distorted thoughts about the cause or consequences of the trauma, leading to persistent self-blame or blaming others.
Emotionally, individuals may feel a constant sense of fear, horror, anger, guilt, or shame. Many report feeling detached or estranged from others, as if they are living behind a glass wall. A key symptom is a markedly diminished interest in activities that were once pleasurable and an inability to experience positive emotions like happiness, satisfaction, or love.
Marked Alterations in Arousal and Reactivity
Finally, trauma can leave the nervous system in a constant state of high alert, as if danger is always imminent. This hyperarousal manifests in several ways.
Individuals are often irritable and prone to angry outbursts with little provocation. They may engage in reckless or self-destructive behavior, such as substance abuse or dangerous driving. A state of hypervigilance is common, where the person is constantly scanning their environment for threats. This is coupled with an exaggerated startle response—jumping at loud noises or unexpected touch.
This state of heightened arousal makes it incredibly difficult to concentrate on tasks or to relax. As a result, problems with sleep, such as difficulty falling or staying asleep, are nearly universal among those with PTSD.
Who Is at Risk for PTSD?
Experiencing trauma is common, but not everyone who goes through a traumatic event will develop PTSD. Several factors can influence a person’s risk. These include the intensity and duration of the trauma, with more severe and prolonged events carrying a higher risk.
A person’s history is also significant. Having a history of previous trauma, especially in childhood, or having a personal or family history of other mental health conditions like anxiety or depression can increase vulnerability. Perhaps one of the most critical factors is the level of social support a person has after the event. A strong, supportive network of family and friends can be a powerful protective buffer.
Evidence-Based Treatments for PTSD
The good news is that PTSD is a treatable condition. Recovery is possible, and several evidence-based treatments have been proven effective. Treatment typically involves psychotherapy, medication, or a combination of both.
Psychotherapy (Talk Therapy)
Therapy is the cornerstone of PTSD treatment. Several specific modalities are highly recommended:
- Trauma-Focused Cognitive Behavioral Therapy (TF-CBT): This is an umbrella term for therapies that focus on how the trauma has affected a person’s thoughts, feelings, and behaviors. Two of the most effective types are Prolonged Exposure and Cognitive Processing Therapy.
- Prolonged Exposure (PE): This therapy helps people gradually and safely confront the trauma-related memories, feelings, and situations they have been avoiding. Through repeated exposure in a therapeutic setting, the fear and anxiety diminish over time.
- Cognitive Processing Therapy (CPT): CPT focuses on identifying and challenging the unhelpful and distorted beliefs that have developed since the trauma (e.g., “It was my fault,” “I can’t trust anyone”). The goal is to develop a more balanced and realistic perspective on the event.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is a unique therapy that involves focusing on the traumatic memory while simultaneously experiencing bilateral stimulation, such as guided eye movements. This process appears to help the brain reprocess the traumatic memory, making it less distressing.
Medication
Medication can also play an important role in managing PTSD symptoms, especially when they are severe. The most commonly prescribed medications are antidepressants, specifically Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs).
These medications can help reduce symptoms of depression and anxiety, improve sleep, and increase concentration. They can make it easier for a person to engage in and benefit from psychotherapy. Other medications may be used to target specific symptoms, such as prazosin for nightmares.
The Path to Recovery
Recovering from PTSD is a journey, not a destination. It requires courage, professional guidance, and strong self-compassion. Beyond formal treatment, developing healthy coping strategies is vital. This includes practicing grounding techniques to manage flashbacks, establishing routines to create a sense of safety and predictability, and leaning on a trusted support system.
Post-Traumatic Stress Disorder is not a sign of weakness; it is a normal reaction to an abnormal experience. It is a testament to having survived something terrible. With the right help and support, individuals can learn to manage their symptoms, process their trauma, and reclaim their lives, moving from a state of merely surviving to one of thriving.